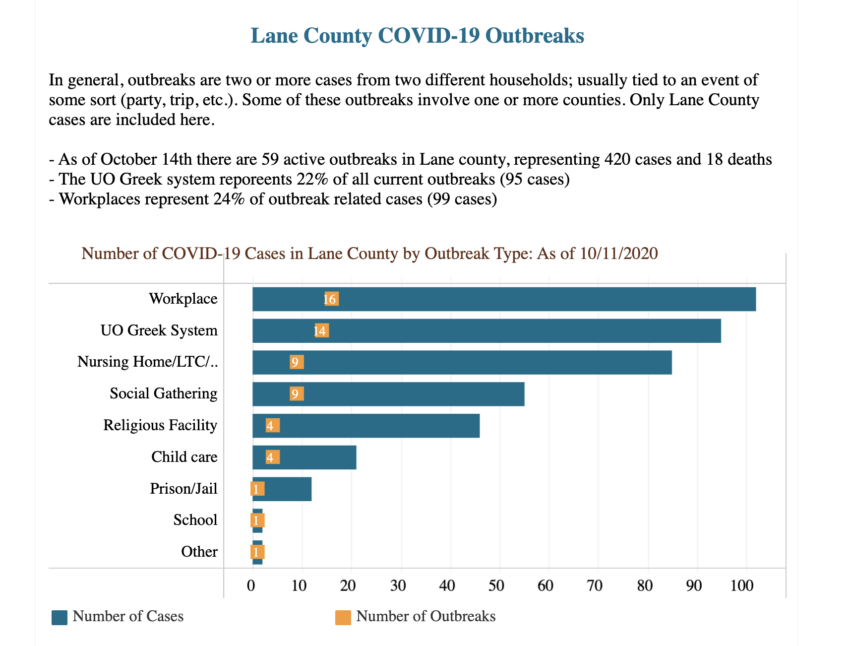
Update – As Thomas Hager helpfully notes in the comments, Lane County Public Health is considerably more transparent than UO. For example, as of 8 days ago, 14 outbreaks in the UO Greek System, with 95 cases, or 22% of all of Lane County’s cases in the preceding week:
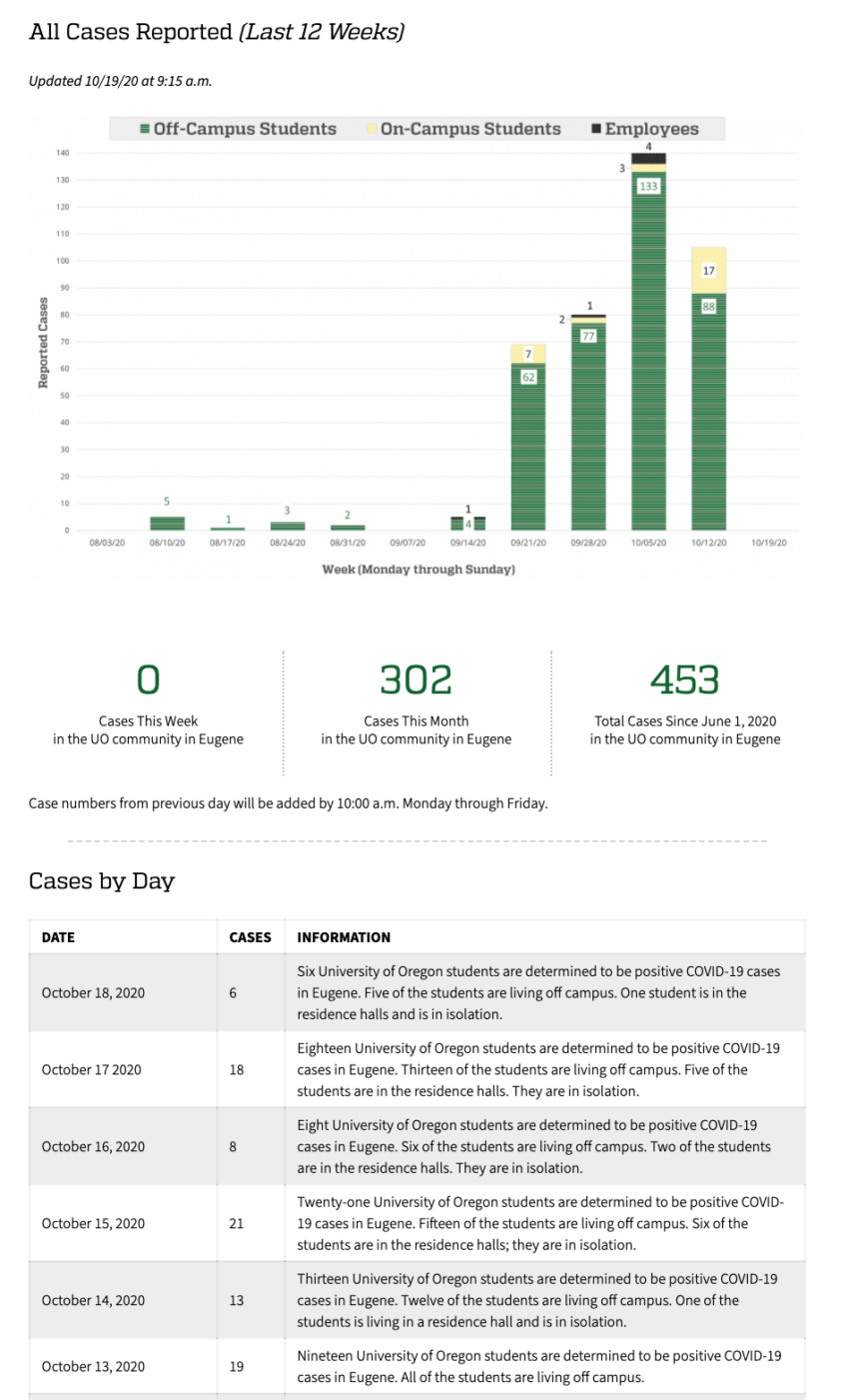
From UO, still no useful information about where the new cases are coming from. Bats? Frats? Athletes? Clusters in specific housing complexes? Big parties? A few here and a few there? Not even a link to the Lane County data above:
Lane County’s Covid-19 website offers a wealth of data. Their many charts (scroll across to find them all) at https://public.tableau.com/profile/lane.county#!/vizhome/LaneCountyCOVID-19WeeklySurveillanceReport/WeeklyReport include one labeled “Outbreak” that says the UO Greek system has been the source of 14 outbreaks leading to 95 cases of the disease. In other news, it appears that college-aged people (18-27) account for the majority of recent cases in Lane County.
Putting these numbers in context: These student cases represent 1/4 to 1/3 of the new cases in all of Lane County during each of the past four weeks. There are about 23,000 UO students (as of last fall, at least), and about 380,000 people in Lane County. Students represent about 6% of the county’s population, but 25-35% of new cases. The UO made a huge mistake in asking the students to come back.
Especially when you consider there is no where near the regular 23,000 students in the Eugene/Springfield area this year. I don’t know that the UO has released any official numbers but I have heard through the grapevine about 2-3,000 in the dorms and a very unofficial estimate of 5-8,000 living off-campus.
That’s also an interesting trendline in the on-campus student numbers hitting two weeks after move-in. If anything forces the UO’s hand, it will be an on-campus outbreak in the dorms.
The owner of a high traffic store estimates to me that 60-70% of the ordnary student population is in town. Somewhat higher than what you are hearing. I wonder how anyone would really know the off campus population.
Yes, but the relevant denominator for college age student Covid cases is college age population, not total population. Making that adjustment puts UO cases still high but more proportionate.
More context: In order for Lane County’s K-12 children to return to in-person instruction, the county needs to have fewer than 40 new cases per week, for three weeks in a row. We were close to that number, and even below it, for a couple of weeks in August, before university students returned to Eugene. Then UO students blew that case number out of the water. UO students’ poor choices are screwing our communities’ children out of a full education and burdening families with supporting in-home schooling. Lane County Public Health says that we should not cast blame at specific groups; I say to hell with that.
https://www.instagram.com/covid.campus/
Don’t know but perhaps the UO is relying on the County as the authority reporting (like they should) instead of actively covering something up (which of course they can’t anyway)
I have yet to hear about any of the 4,000 weekly tests Schill touted last week.
Meanwhile, football players are tested daily.
https://www.registerguard.com/story/sports/college/football/2020/10/19/pac-12-announces-covid-19-thresholds-cancellations-tiebreakers/5982482002/
Why the focus on number of “cases”? It’s been shown that ~90% of people testing positive have no symptoms (asymptomatic or not infected at all) (https://www.nytimes.com/2020/08/29/health/coronavirus-testing.html). Of the students testing positive (from this so-called outbreak) how many are actually sick, hospitalized, or have died??
If you look at the website (see the first link in the commentary above) under the “targeted testing” tab they report that “88% of those cases reported at the time of testing that they had no symptoms.”
The CDC data on excess deaths (https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm) is a good way to see how the country and individual states are doing compared to average. Excess deaths for the country as a whole and Oregon as a state have dropped below the threshold for excess deaths for this time of year. What does this mean? This means the pandemic is over.
If you do want to track cases, it should be reported as a percentage of positive tests given the number of tests performed and the meaning of a positive test result should be explained.
The pandemic is over, are you kidding? Go to worldometers, 700 or so covid deaths daily in U.S. Experts, yes, they are not all idiots, project 170,000 more deaths by Jan 31, almost 400,000. I know that NYT article, it does not mean what you think.
Symptomatic or not, people who test positive are likely to infect others, spreading the disease faster and upping the eventual number of deaths. Case numbers are vital in tracking and, if possible, controlling this spread. Saying “the pandemic is over” is ridiculous.
It’s extremely hard to tell what counts as a COVID death. If you look at the Oregon Heath Authority reports, for example, pretty much all of the deaths are listed as having underlying conditions. It’s not at all clear what is actually the cause of death. Did COVID contribute to the death or did the person die of a primary non-COVID related issue and happened to test positive for COVID, so they were counted as such? It’s impossible to tell from the information provided. The CDC does not require such accounting. Since March 24th the CDC also doesn’t require a COVID test to count a case as a COVID death. This is why looking at all-cause mortality is useful to assess the actual situation. As such, it suggests that death rates are back to normal.
The PCR test is extremely problematic as a diagnostic test, especially the way it is being implemented with 35 to 40 cycles of amplification of genetic material. A positive test doesn’t mean that someone is infected or will infect others.
Contact tracing and epidemiological studies have shown that healthy people (including those who test positive but are asymptomatic) do not drive the spread of the virus (https://www.cnbc.com/2020/06/08/asymptomatic-coronavirus-patients-arent-spreading-new-infections-who-says.html; http://www.emro.who.int/health-topics/corona-virus/transmission-of-covid-19-by-asymptomatic-cases.html). The evidence suggests that spreading is occurring from symptomatic patients who are in close contact with others.
You really seem to be suggesting that nobody is dying from covid now. But reports are close to a thousand daily deaths. I don’t believe you know what you are talking about. Can you link to any expert source that makes your argument?
The overall COVID death rate is slowly in decline – this is said and documented by virtually every agency and was on NPR yesterday.
Many reasons are contributing to this
https://www.theatlantic.com/ideas/archive/2020/07/why-covid-death-rate-down/613945/
is a good synopsis although done in July.
The ratio of deaths to new cases (including lag time) is definitely
lowering, so that is good news.
Thanks for the link. Here’s another link that tracks the time course of COVID (https://www.youtube.com/watch?v=8UvFhIFzaac). It shows that: 1) the COVID time-course and impact is similar to past influenza epidemics. 2) There is a lack of an effect of lockdowns and mask use on outcomes of COVID. Four decades of research have shown that masks are not effective in stopping respiratory viral transmission. During the COVID epidemic, mask use has had no impact on COVID outcomes. 3) An important factor influencing the impact of COVID in different regions is the severity of the prior flu season (inverse correlation between severity of prior flu season and severity of COVID). 4) Seasonality. There are two time courses for COVID that depend on climate. The same pattern happens for the flu. An early sharp pattern of deaths that occurs in “temperate” climates (Europe, NE US, Mid-West US) and a delayed, more extended pattern of deaths that occur in “tropical” climates (Brazil, Peru, Mexico, Southern US, West US). This accounts for the so-called “second wave” which is simply due to the delayed peak in deaths in “tropical” climates. 5) Casedemic: Hyper testing with PCR results in a dissociation between number of cases and deaths – huge numbers of cases and dwindling deaths. This is what we are seeing now. 6) Finally, a worry that locking down during periods of low death rates may decrease population immunity, possibly causing an increase in death rates (for flu and corona viruses) in the Winter.
The CDC thinks mask use cut Arizona cases by 75%. https://www.cdc.gov/mmwr/volumes/69/wr/mm6940e3.htm
Nature says masks are effective: https://www.nature.com/articles/d41586-020-02801-8
I don’t get the climate argument given that North Dakota and Florida are both seeing increased cases as well as much of Europe and Argentina and Israel are all seeing surges. What “climate” is spared right now?
A lot of the studies referenced in the Nature article are anecdotal observational accounts (e.g., spreading not occurring at outdoor rallies attributed to mask wearing … it’s been shown that spread is lower in outdoor settings masks or no masks), comparing rates before and after masks are mandated, or different regions with or without mask mandates. The tests that need to be done, which I don’t see in that article, are randomized controlled trials (https://www.meehanmd.com/blog/2020-10-10-an-evidence-based-scientific-analysis-of-why-masks-are-ineffective-unnecessary-and-harmful/).
The CDC website shows that the excess death rate in Florida continues to decline. North Dakota does have an up tic in excess deaths, though it really didn’t have much of a peak earlier (in April). Again, in many places the spike in cases (positive tests) is not related to a spike in illness or deaths.
Here are RCT mask studies for you for respiratory viruses, Dark Star:
https://www.ijidonline.com/article/S1201-9712(08)01008-4/fulltext
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7191274/
If you are looking here https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm
Then you need to be very careful in the interpretation. As the site notes, the numbers for the previous 8 weeks are incomplete and get revised as the death certificates are coded and submitted. Florida in particular has many deaths that occurred weeks before the report date because they are slow and backlogged, so Florida’s dashboard always shows deaths, excess deaths and cases on the decline.
I looked at the first link and found this in the first paragraph “However, there are no prospective randomised control trials on face masks in prevention of viral respiratory infections”. This is a patently false statement!
The second link pretty much dismisses the 20+ years of randomized control trials on face masks in the prevention of viral respiratory infections:
“Many systematic reviews have been conducted on masks, respirators and other PPE in past (Cowling et al., 2010; Bin-Reza et al., 2012; Gralton and McLaws, 2010; Gamage et al., 2005; Jefferson et al., 2009; Jefferson et al., 2011; Jefferson et al., 2008; Aledort et al., 2007; Lee et al., 2011; Verbeek et al., 2020). These reviews generally examined multiple interventions (e.g. masks and hand hygiene etc.), often combined different outcome measures that were not directly comparable and were inconclusive. Moreover, most of these reviews did not include more recent randomised controlled trials (Radonovich et al., 2019, MacIntyre et al., 2015).”
These RTCs and meta analyses were far from “inconclusive” (see below for a few samples).
This purposeful ignoring/mischaracterization of the ample literature is weird, unfortunate and scary.
——————————————
Jacobs, J. L. et al. (2009) Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: A randomized controlled trial, American Journal of Infection Control, Volume 37, Issue 5, 417-419.
https://urldefense.com/v3/__https://www.ncbi.nlm.nih.gov/pubmed/19216002__;!!C5qS4YX3!QiWF3RFxEGIJ8ptMmMGgJSxI6QclebbrLPKr_nwg72N_bRagsqTZYzc4xgpoW_SQ$
N95-masked health-care workers were significantly more likely to experience headaches. Face mask use in health-care workers was not demonstrated to provide benefit in terms of cold symptoms or getting colds.
————————————————————–
Cowling, B. et al. (2010) Face masks to prevent transmission of influenza virus: A systematic review, Epidemiology and Infection, 138(4), 449-456.
https://urldefense.com/v3/__https://www.cambridge.org/core/journals/epidemiology-and-infection/article/face-__;!!C5qS4YX3!QiWF3RFxEGIJ8ptMmMGgJSxI6QclebbrLPKr_nwg72N_bRagsqTZYzc4xrpoZBfQ$ masks-to-prevent-transmission-of-influenza-virus-a-systematic- review/64D368496EBDE0AFCC6639CCC9D8BC05
None of the studies reviewed showed a benefit from wearing a mask, in either health-care workers or community members in households (H). See summary Tables 1 and 2.
————————————————————–
bin-Reza et al. (2012) The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence, Influenza and Other Respiratory Viruses 6(4), 257–267.
https://urldefense.com/v3/__https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1750-2659.2011.00307.x__;!!C5qS4YX3!QiWF3RFxEGIJ8ptMmMGgJSxI6QclebbrLPKr_nwg72N_bRagsqTZYzc4xtBLbNLJ$
“There were 17 eligible studies. … None of the studies established a conclusive relationship between mask/respirator use and protection against influenza infection.”
————————————————————–
Smith, J.D. et al. (2016) Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis, CMAJ Mar 2016, cmaj.150835;
https://urldefense.com/v3/__https://www.cmaj.ca/content/188/8/567__;!!C5qS4YX3!QiWF3RFxEGIJ8ptMmMGgJSxI6QclebbrLPKr_nwg72N_bRagsqTZYzc4xhhVXr-I$
“We identified 6 clinical studies … In the meta-analysis of the clinical studies, we found no significant difference between N95 respirators and surgical masks in associated risk of (a) laboratory-confirmed respiratory infection, (b) influenza-like illness, or (c) reported work-place absenteeism.”
————————————————————–
Offeddu, V. et al. (2017) Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis, Clinical Infectious Diseases, Volume 65, Issue 11, 1 December 2017, Pages 1934-1942.
https://urldefense.com/v3/__https://academic.oup.com/cid/article/65/11/1934/4068747__;!!C5qS4YX3!QiWF3RFxEGIJ8ptMmMGgJSxI6QclebbrLPKr_nwg72N_bRagsqTZYzc4xlgbUQ1A$
“Self-reported assessment of clinical outcomes was prone to bias. Evidence of a protective effect of masks or respirators against verified respiratory infection (VRI) was not statistically significant”, see Fig. 2c.
————————————————————–
Radonovich, L.J. et al. (2019) N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial, JAMA. 2019; 322(9): 824-833.
https://urldefense.com/v3/__https://jamanetwork.com/journals/jama/fullarticle/2749214__;!!C5qS4YX3!QiWF3RFxEGIJ8ptMmMGgJSxI6QclebbrLPKr_nwg72N_bRagsqTZYzc4xn1-GGaH$
“Among 2862 randomized participants, 2371 completed the study and accounted for 5180 health-care workers-seasons. … Among outpatient health care personnel, N95 respirators vs medical masks as worn by participants in this trial resulted in no significant difference in the incidence of laboratory-confirmed influenza.”
————————————————————–
Long, Y. et al. (2020) Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis, J Evid Based Med. 2020; 1-9.
https://urldefense.com/v3/__https://onlinelibrary.wiley.com/doi/epdf/10.1111/jebm.12381__;!!C5qS4YX3!QiWF3RFxEGIJ8ptMmMGgJSxI6QclebbrLPKr_nwg72N_bRagsqTZYzc4xt04MpAz$
“A total of six RCTs involving 9 171 participants were included. There were no statistically significant differences in preventing laboratory-confirmed influenza, laboratory-confirmed respiratory viral infections, laboratory-confirmed respiratory infection and influenza-like illness using N95 respirators and surgical masks. Meta-analysis indicated a protective effect of N95 respirators against laboratory-confirmed bacterial colonization (RR = 0.58, 95% CI 0.43-0.78). The use of N95 respirators compared with surgical masks is not associated with a lower risk of laboratory-confirmed influenza.”
There are a number of things being tossed into this discussion. I think it’s important to separate flat or decreasing death rates (rooted in treatment improvements) from increasing incidence rates (rooted in poor public health practices). We should celebrate medicine’s ability to keep death rates down, and focus on keeping incidence rates low as well so we don’t swamp the healthcare system. Wear your mask, keep distanced, and avoid large gatherings indoors — using these common-sense measures can get us through until we have an effective vaccine.
Yes, the decreasing death rates are due in part to treatment improvements but also to the normal waning of the effects of the virus. This virus is no different from other viruses in that respect. A vaccine would be great to help boost population immunity, but can be dangerous if rushed. There are other effective and cheap treatments — e.g., large vitamin D doses on admission with a 25x reduction in ICU admissions (http://www.rationaloptimist.com/blog/britains-vitamin-d-deficiency) and hugely effective, standard steroid inhalers that are already routinely available in all ERs (https://markcrispinmiller.com/2020/10/how-to-empty-every-icu-of-all-covid-19-patients-in-48-hours-must-watch/). We should also be cognizant of the terrible toll the lockdowns have caused — an estimated ~100,000 excess deaths in the US (https://www.cdc.gov/mmwr/volumes/69/wr/mm6942e2.htm?s_cid=mm6942e2_w).
Dear Dark Star, Since early April I have been following the COVID story at the CDC website here:
https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm
I agree with your analysis. I’ve been widely derided for my position that COVID is, at it’s core, a Dog Wag/False Flag play on the global scale. Venture now to say the numbers most important to understand may be expressed in currency.
A note to commenters:
.
While the comment form asks for an email address, if you leave that blank or make up something silly the software will still accept your comment. While the mail addresses are not posted, I can see them in the admin comment screen.
.
I would prefer that people not enter a real email address, unless they have some reason to want me to know it. A fake but consistent email address is a good idea if you are worried that someone might misuse your screen name – it serves a way for me to know that a comment comes from the person regularly using that name.
.
Thanks, UOM
UOM, Every single time I have tried to send a comment without an email address, it fails to post. After about a dozen failures, I started to include an email address, and all of those have posted. So I’m a little skeptical that they post without an email address.
Hmm, OK, that’s weird because I get plenty of comments with no email address. BTW, nicely chosen fake one.
[UOM: I’ve deleted this comment, out of privacy concerns for the family.]